Why do certain mutations in key genes predispose someone to particular types of cancers?
August 15, 2012
An undergraduate from the U.S. asks:
"I have a friend who has Hereditary Non-Polyposis Colon Cancer (HNPCC). In this hereditary disorder there is an error in one or more DNA repair genes (specifically mismatch repair). This mechanism - mismatch repair - is used throughout the body.
So my question is: why does this inherited error predispose the person to cancers of the colon and not of other tissues? Similarly, for BRCA-related cancers: why the predisposition to breast and ovarian cancer? Another to add to the list is retinoblastoma. Why does a defect in the Rb gene lead specifically to a higher risk for an eye cancer and not a generalized increased risk of any cancer?"
The short and sweet answer is that some genes are more important in certain types of tissues. For example, genes involved in sight are obviously going to be more important in your eyes than in your colon.
But this explanation is a little harder to understand with the genes we are talking about. As you point out, they are involved in important things that every cell does.
What probably makes them affect certain tissues more than others is how different cells use them. And how they interact with different genes in each cell.
A good example is retinoblastoma and the Rb gene (which you mentioned). Every cell uses the Rb gene, so it clearly has a job important for the whole body. But when Rb gets damaged, cancer is more likely to happen in a specific part of the body — the retina of the eye.
We aren’t positive about why this is the case, but we do have a good theory. It has to do with a couple of genes called p130 and p107.
In most cells, p130 and/or p107 can be used as backups when Rb breaks. They can step in and take care of the jobs Rb usually does. These tissues are protected from the effects of a broken Rb.
The same is not true in the retina. For some as yet unknown reason, cells there can’t use these other genes as a replacement for Rb. So when Rb breaks, the retina becomes especially likely to get cancer.

We don’t know as much about breast and colon cancer as we do about retinoblastoma. However, it’s very likely that the story behind most hereditary cancers, including breast and colon, will be very similar to the case of Rb and retinoblastoma.
I’ve given you a short and sweet answer to this question, but it leaves a lot of information out of the picture! To understand the full story behind these hereditary cancers, we need to take a quick refresher on how cancer happens.
DNA Changes Cause Cancer
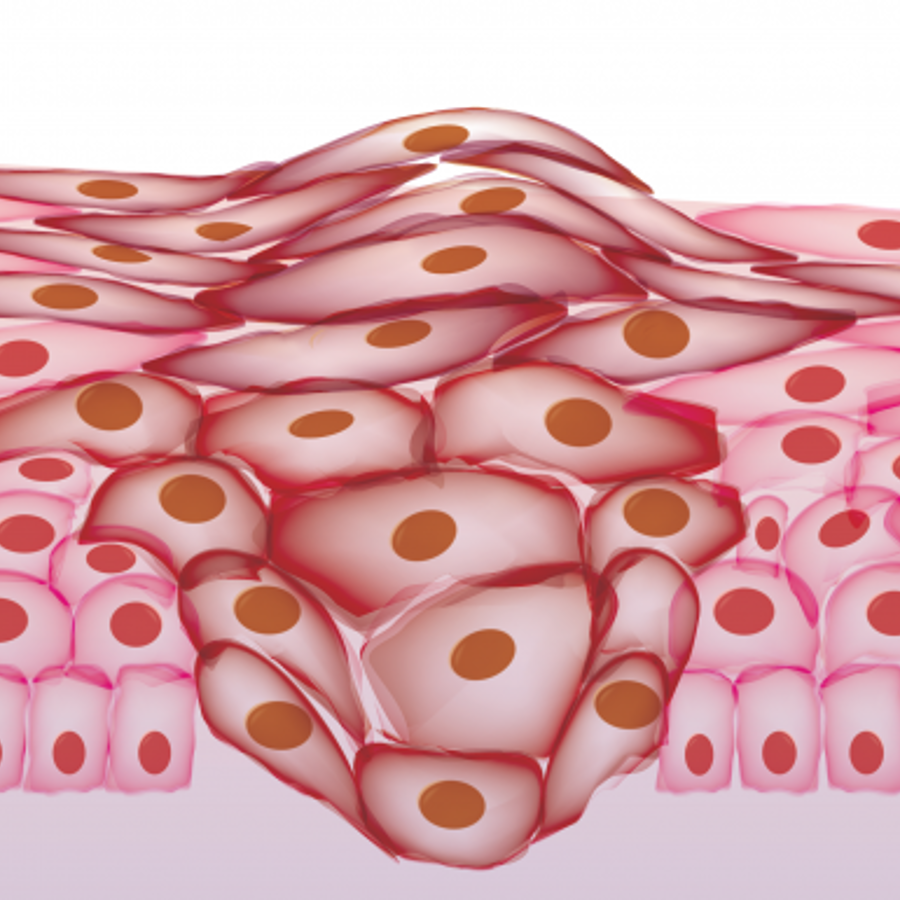
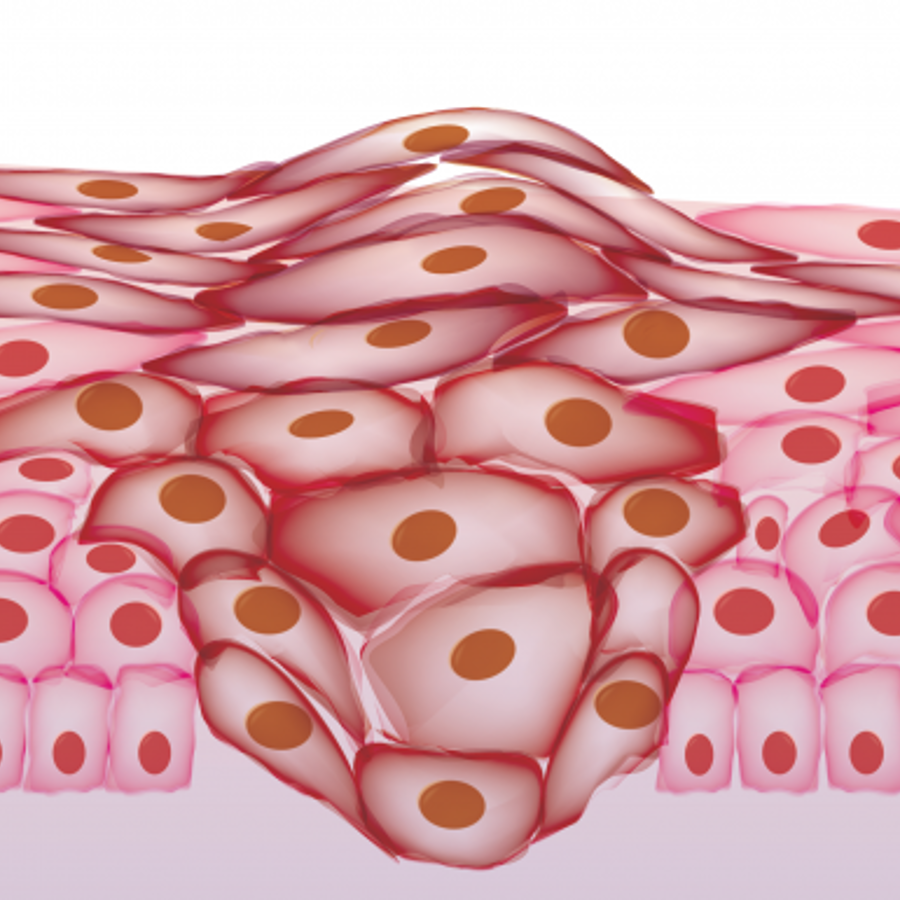
Cancer is a bunch of cells in your body that have stopped following the rules. These cells will just grow and grow until they become a danger to your health. In the end you have to destroy them to survive.
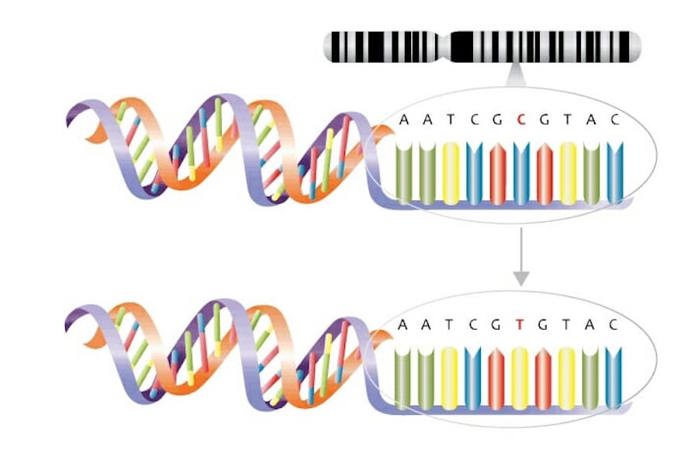
Cells turn cancerous because of mutations in the DNA of important genes. For example, mutations in genes that tell your cells when to grow, when to stop growing, and/or when to die can all make a cell go rogue.
Genes can get mutated in a couple of different ways. One way is when something from the outside world damages it. This is how UV rays from sunlight can lead to skin cancer and how chemicals in cigarette smoke can lead to lung cancer.
The other way to mutate your genes is when a cell accidentally mutates its own DNA. This can happen whenever a cell divides.
Cell division is the way that our body makes new cells — it takes one cell, doubles everything inside of the cell, and then divides it into two cells. In this process, the cell also needs to copy all six billion letters of its DNA. It is during this copying that a mutation can creep in.
If you’ve ever had to copy a bunch of text by hand and made a few mistakes, you know what happens when a cell copies its DNA. You also know what happens if you’ve ever played the game Telephone.
In Telephone, one person whispers a sentence into someone's ear. The words are then whispered from person to person around a circle. By the time the last person says the words out loud, the sentence can get pretty bungled!
It’s the same way with cell division. The more times you need to copy your DNA, the more chances there are to make a mistake. This is why cancer usually happens in tissues that do a lot of cell division, like breast and colon. It’s also why older people get cancer… they’ve had more cell divisions and so are more likely to have mutations in important genes.
Luckily, most mutations are harmless. And we have two good built-in safeguards to deal with mutations that might cause problems. One is to fix the mutation, and the other is to kill the cells that have just gotten new mutations.
The genes you mentioned in your question are great examples of safeguards. The Rb gene controls cell division and can remove mutated cells by allowing them to die. The BRCA1/2 genes and the DNA mismatch repair genes fix certain types of damaged DNA.
You get in trouble when these safeguard genes break. Mutations can’t be fixed as well, which means that you’ll end up with more mutations. And the more mutations you have, the more likely one is to hit something important.
Different Tissues, Different Problems
Now we are finally ready to tackle your question. We’ve already gone over retinoblastoma and the Rb gene. But that still leaves breast cancer and the BRCA1/2 genes, and colon cancer and DNA mismatch repair genes.
We don't know the full answer yet as to why mutations in these genes affect certain tissues more than others. But we do have some good ideas.
In the case of breast cancer, we know that BRCA1/2 is important for fixing damaged DNA. However some scientists think that it might have another role too. This second role is controlling estrogen, which is a hormone that tells certain cells to divide. It basically sends a ‘grow!’ signal to these tissues.
Estrogen is best at making tissues like breast and ovary grow. One theory is that the loss of BRCA1/2 causes these tissues to grow because of an increase in estrogen. Remember, more cell divisions mean more mutations.
So when BRCA1/2 is damaged, you get a double whammy. Cells sensitive to estrogen start collecting mutations as they divide more, and they also cannot fix these new mutations.
This is just a theory at this point. But scientists are doing experiments right now to try and sort out whether this is happening.
We don’t know as much about why DNA mismatch repair genes are important to HNPCC (Hereditary Non-Polyposis Colon Cancer). But scientists of course have a few ideas!
A common kind of DNA mistake is called a mismatch. There are a bunch of genes that specifically fix this type of mutation.

When these mismatch repair genes are damaged, people can end up with colon cancer. One theory to explain this is that mismatch mutations tend to happen in genes specific for colorectal health.
This would mean that when you lose a mismatch repair gene, mismatch mutations build up throughout your body. But, the colon has key genes that are more sensitive to these kinds of mutations. When these genes are damaged in the colon, you are more likely to get cancer there.
Remember, this is just one of many theories at this point. We need to do much more research to truly understand what’s going on.
I hope I’ve helped to shed light on this complicated question — this is a very exciting field that promises to reveal some awesome insights into human biology!
Read More:
- American Cancer Society: A bit about genes that are important in cancer
- National Breast Cancer Foundation: More about what BRCA genes do and why it’s dangerous when they’re mutated
- Scitable: Why one mutation is usually not cancer-causing

Author: Zoe Assaf
When this answer was published in 2012, Zoe was a Ph.D. candidate in the Department of Genetics, studying evolution and genomics in Dmitri Petrov’s laboratory. She wrote this answer while participating in the Stanford at The Tech program.
 Skip Navigation
Skip Navigation
